Improving outcomes for IBD in 2022
Early effective therapy, treat-to-target, pros & cons of anti-TNF, new small molecules and holistic patient-centered care
There are many simple and cost-effective measures that we can implement at scale, right now to improve outcomes in IBD.
We have previously described and discussed the the urgent unmet need in IBD.
Some of these needs may be out of immediate reach. We will need to maintain and indeed accelerate current R&D spending in IBD. The necessary clinical trials will take time to deliver. Many important RCTs of new therapies, combinations of therapies and paradigm-busting treatment strategies are underway or being planned.
What we do have now is an effective therapeutic toolkit.
We also possess a robust treatment framework, thanks to pivotal strategic studies with existing and new molecules. Additionally we have a deeper appreciation of the impact IBD has on a person’s life and tools we can use to address this - dietary, psychological, behavioural, social.
Let’s dive in.
1. Early effective therapy in Crohn’s disease
The clock starts ticking at diagnosis of Crohn’s disease and probably before.
Treating Crohn’s disease effectively, early in the disease course results in better outcomes. Effective therapy in 2022 means a biologic. Biosimilars make this cost-effective using an anti-TNF based treatment strategy at scale.
We do have one problem.
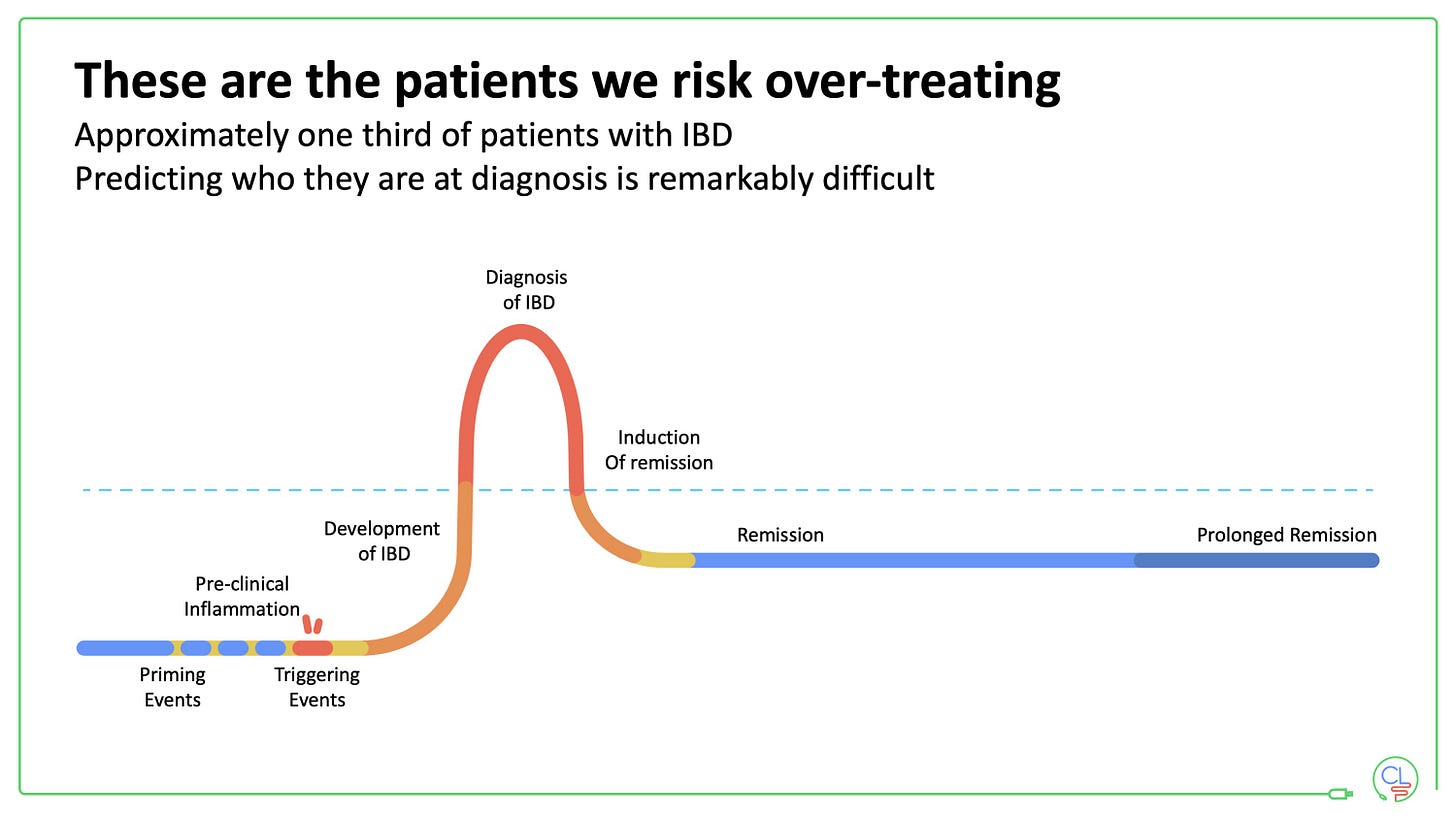
\Whilst for some patients it is clear that early anti-TNF is indicated (extensive small bowel disease, fistulising disease, deep ulcers at endoscopy) for many others it is hard to predict complicated outcomes from the point of diagnosis. We risk over-treating the one third of patients who will have a quiescent disease course.
Our pragmatic solution to this is as follows:
Choose which patients to start on anti-TNF from the outset
For those with mild-moderate disease and without risk factors, give induction therapy (e.g. budesonide / enteral nutrition) and monitor
Lifestyle advice: stop smoking, dietary changes (for now a Mediterranean style diet is probably best)
In these patients check calprotectin every 2m for at least year 1
If calprotectin normalises in year one (<250mcg/g) then continue on no maintenance therapy
If calprotectin remains above 250mcg/g then start a biologic
We use IFX and AZA for high-risk patients and often ADA monotherapy with proactive TDM (high vigilance for emerging immunogenicity)
2. Expedient management of flares in UC
The way to minimise steroid use, avoid admissions and reduce colectomy rates in UC is by expediently managing disease flares.
I set up a flare clinic in the pandemic – our solution to see the patients we needed to see early, when the routine clinics were shut / virtual.
This is how our flare clinic works:
Patient phones IBD nurse helpline or GP contacts IBD team
Wonderful IBD nurses triage calls first thing in morning and contact patients
Daily team huddle on zoom at 10am: consultant led decision making
Patients triaged to advice, admissions, routine / urgent clinic or flare clinic
Same day review at flare clinic – one to two patients only
Consultant plus IBD nurse plus / minus pharmacist and dietitian
Assess, examine, labs, biologic screening, stool sampling, advanced therapy counselling, prescribing and dispensing or booking infusion appointment
This ensures patients who need therapy don’t wait unnecessarily. Our system is not perfect and very busy so there is a wait (maybe four weeks) for more routine biologic starts.
Small molecules fit very nicely into this paradigm.
Rapid onset of action, dispense from hospital pharmacy SAME DAY and no need for corticosteroids. Currently we use tofacitinib, but this will evolve with the imminent arrival of two new JAK1 selective inhibitors.
We have a serious of interesting drug positioning / sequencing questions in UC with all this new choice of therapies. But let’s not get too distracted with that for now. Adopting established treatment frameworks are more important. Starting an effective therapy early in a flare is the main step that will improve outcomes.
Final point on UC: work closely with surgical colleagues and involve them early in patients who are not responding to medical therapy.
3. Appropriate use of treat-to-target with non-invasive monitoring tools
Treat to target works in theory AND in practice.
REACT and CALM demonstrated this. STRIDE-2 gives us the framework. Whilst colonoscopy is the gold standard for mucosal assessment, faecal calprotectin and point-of-care intestinal ultrasound (POCUS, not to be confused with POTUS) provide robust non-invasive monitoring tools
We use calprotectin a lot.
The same assay has operated in our lab since 2005, running well in excess of 100,000 ELISAs. We test at every clinical interaction and every 2m in high-risk situations: new diagnosis, new advanced therapy start and / or stop, post-surgery. This allows longitudinal comparisons.
Calprotectin testing is based on an ELISA. It should be very cheap – we pay approx. £10 per assay. If you are paying more then stop and ask WHY??? I do not think current point-of-care calprotectin tests are reliable or cost-effective enough to recommend widely.
This box is from the recent review that Nik Plevris and I wrote on disease monitoring for IBD in Gastroenterology.
People who have adopted point-of-care ultrasound (POCUS) love it.
I can understand this. Rapid, patient friendly assessment of mucosal and transmural inflammation and complications in the clinic.
We do not use POCUS yet.
We have fantastic calpro and small bowel MRI services that we rely on. And the NHS is not a straightforward place to enable the necessary training and deployment. But we are working on this now.
Whatever tools you have available, using them as part of a treat-to-target strategy is the best way to optimise treatment outcomes for patients.
4. Recognise the pros and cons of anti-TNF drugs
Anti-TNF drugs are highly effective in IBD, but they are not without fault.
At least 30% of patients will not respond (primary non-response), 20% of initial responders will develop immunogenicity and stop within a year, and 10-15% will do similarly each subsequent year.
So the drug persistence is terrible – especially with monotherapy, in obese and overweight patients, smokers and carriers of the HLA-DQA1*05 risk haplotype. Infliximab is the worst for this in it’s intravenous form – subcut infliximab (with CT-P13) may be better as a monotherapy agent. Anti-drug antibodies to adalimumab are also a problem.
The next problem is drug sequencing.
After TNF failure other drugs work less well. This is especially true for vedolizumab and ustekinumab. In our study of 150 patients with Crohn’s disease treated with USTE after prior TNF, 30% needed escalating to 4 weekly therapy within 1 year.
New small molecules will hopefully get around this issue to an extent.
We already see this in the clinic with tofacitinib in UC. The data look very promising for upadacitinib in Crohn’s disease with or without prior TNF failure.
For now the data and cost continue to support starting with an anti-TNF based strategy in Crohn’s disease, but it is less clear cut in UC.
5. Think holistically with patient-centered care
People living with IBD have to content with physical and psychological features and an impact on many aspects of everyday life.
We need to be creative here, and also realistic. This is one area where there are big inequities in care and resource provision.
I’d like to encourage clinicians to ask our patients some simple questions:
What is on your agenda today?
How are you?
What is your sleep like at the moment?
How are your energy levels?
Is there anything you can’t do just now because of your IBD?
How is your diet?
Are there foods that you are avoiding because they trigger symptoms?
How is your mood?
Are you having an issues relating to intimacy?
I aim to ask a variation of these questions in most clinical interactions.
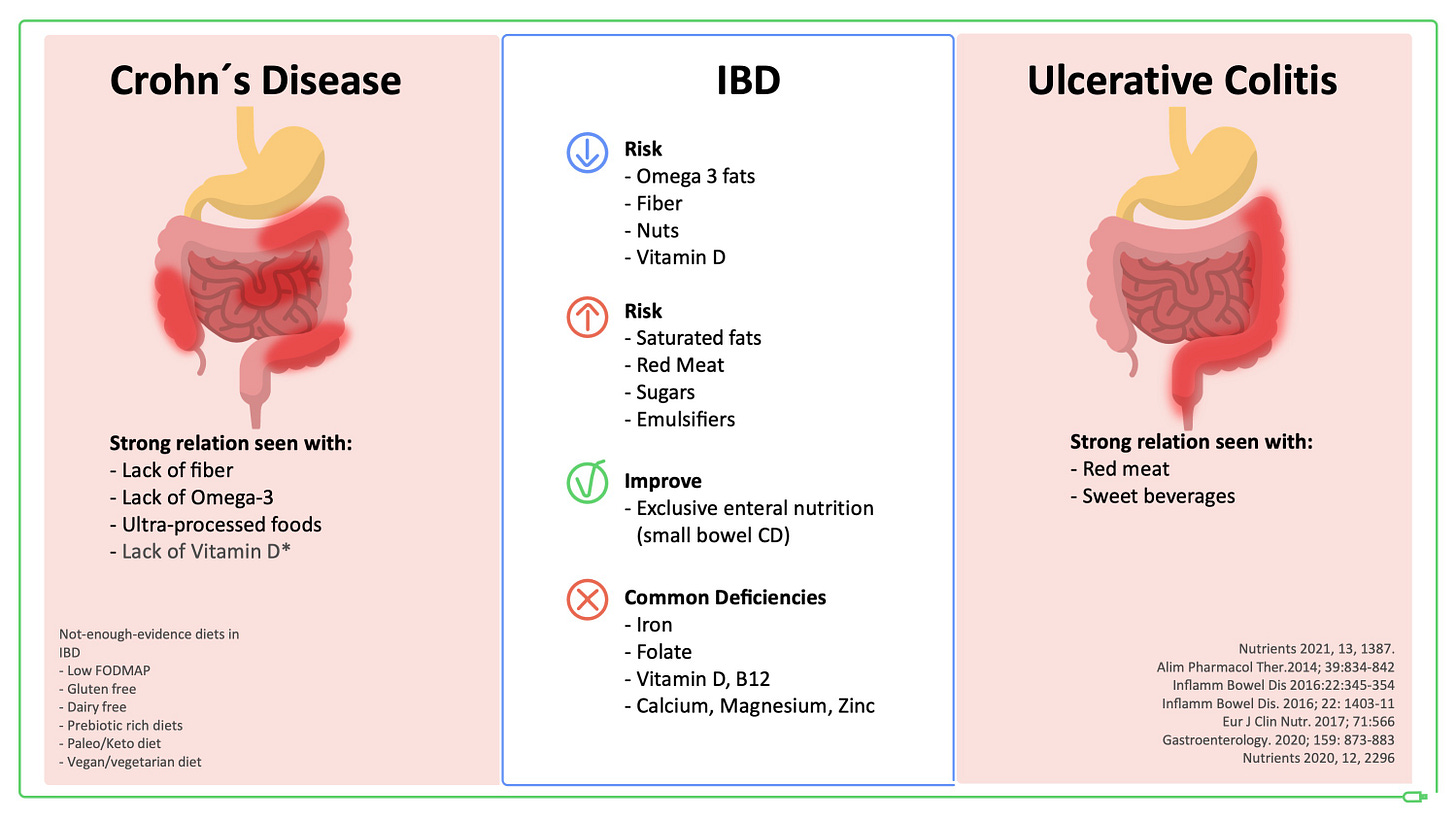
This panel (below) is from a recent IOIBD consensus on “Lifestyle, behaviour and environmental modification for the management of people with IBD” published in Lancet Gastro Hepatology.
Many clinicians tell me they don’t ask because they don’t know what do say and they don’t feel like they can provide solutions to these problems.
Some of this is true. Some of it is avoidance.
Patients tell us that often they are happy just to be asked about these areas and to have their problems / concerns listened to. They recognise there may be a limit to what we can do.
I often give simple lifestyle advice myself in the clinic.
I talk about systems to help with sleep routines, exercise, daylight / nature exposure (to improve mood and energy levels) and mental well-being.
I will also discuss dietary strategies. I aim to fit these with an individual patients needs and circumstances. We have wonderful dieticians but they are too over-stretched to give most patients with IBD dietary advice.
Anxiety and depression are common in people living with IBD.
If I or a patient is worried about their mood I will encourage them to phone their GP the same day. Many GPs offer excellent and very responsive services to help people with mental health issues.
I would dearly love to have psychologists firmly embedded within out clinical service but we do not have this resource. In fact there are not enough qualified clinical psychologists in the UK, so it is not simply a matter of funding.
For now the message is do what you can and do it promptly.
There is an increased risk of severe harm, including suicidal ideation and completed suicide in IBD – in a recent Scandinavian study this was demonstrated in the first year after a new diagnosis of Crohn’s disease (Ludvigsson J et al Journal of Crohn's Colitis 2021.
To our patients, please hang in there and talk to us – or to someone – if you are feeling low or anxious.
Summary:
Awareness and education are key to improving outcomes in IBD with what we have.
Our medical workforce is burnt out and overstretch after the pandemic. Our patients with IBD have many unmet needs, of which several are urgent. Co-ordinated strategies, investment of money and time are required to tackle our bigger goals of prevention and cure.
But thankfully there is a lot we can do today to improve outcomes for many people living with IBD.
So please continue to have hope. Hope is a powerful medicine.








Thanks a lot Charly! I am a ped Gastro in Chile. And we are seeing a huge rise in the incidence of Pediatric IBD here. Your comments and recommendations are a gift! I Also add to the Holistically view of the disease. We need to spend part of our time in these topic, for sure our patients will improve.
Thanks. That was super helpful.