There remains an urgent unmet need in IBD.
Rates of Crohn’s disease and ulcerative colitis continue to rise globally. We are now talking about and researching prevention strategies, but these will take time to arrive. Meantime patients have unequal access to expert care, latest medicines, nursing, dietary and psychological support.
These are key areas of urgent unmet need for IBD in 2022:
Raising awareness
This needs to happen across ALL areas in public, in healthcare, to policy makers, funders and employers.
It needs to happen globally and across all areas of society.
Ensuring equity of IBD care
IBD can affect anyone.
Incident rates are highest in younger people. These young people grow old with IBD. Remember we have no known cure.
IBD does not care if you are black or white, rich or poor. Increasingly IBD does not care where you live in the world. Nor does it care if you have access to expert medicine care.
We must ensure everyone has access to high quality IBD care.
Stratification of patients
A one sized fits all approach does not work in IBD.
We only have relatively few methods by which we can stratify our patients. Young age, extensive disease, deep ulcers, fistulas and smoking are associated with bad outcomes in Crohn’s disease. But we’ve known this for 20 years and urgently need more and better.
Who will have aggressive versus quiescent disease? Know this and we can avoid the common traps of both OVER and UNDER treatment.
Who is at risk from the complications of the disease and of the therapies we use to treat it?
Who will response to what therapy and when?
The holy grail is precision medicine - sorely lacking to date in IBD.
This is a HARD problem. Some have grown very skeptical. I remain optimistic but this will take massive investment in large scale single sequencing experiments. IBD is complex and we need to get the resolution of individual cell types to study drug effects.
We need large coordinated experiments with high throughput translational pipeline with a huge investment from funders, academics, clinicians and patients.
Breaking through the therapeutic ceiling
Current therapies are very effective in some people when used at the right time. We now have an excellent therapeutic toolkit, much of which is not crazy expensive.
But most max out at about 40% steroid free clinical remission at 1 year with slightly lower mucosal healing rates.
What is the solution?
newer more targeted therapies
combinations of therapies
predictive tools
microbial and dietary therapies
Microbial and dietary therapeutics
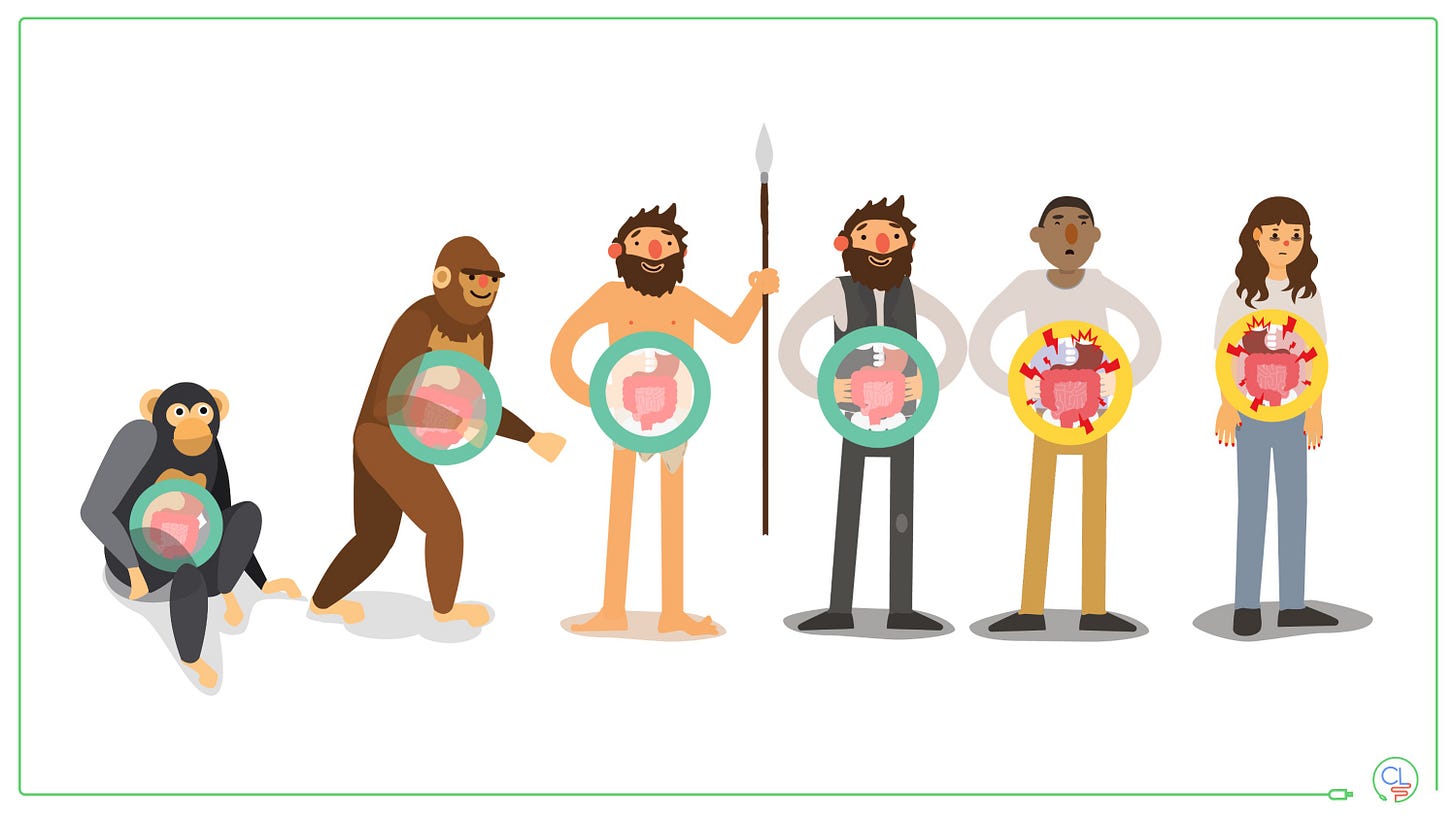
There is compelling evidence for a strong role of diet and the gut microbiome in IBD pathogenesis.
But the precise role is unclear and simple labels like “junk foods cause Crohn’s disease” are unhelpful and not true. I look after many patients who have always had extremely healthy diets.
Nonetheless dietary and microbial strategies to treat active IBD and to maintain remission are highly likely to come to the clinic in the next 5 to 10 years. We need rigorous longitudinal data to build the evidence basis around the role of diet and microbiome in IBD - the GEM project and my PREdiCCt study will provide key insights here.
Next we need to hold dietary and microbial therapies to high standards of clinical trials just as if they were investigational medicines. The DINE study has shown that a randomised head-to-head study of two dietary strategies can be performed and will yield meaningful data.
Effective therapies for fistulas and strictures
These are areas of huge unmet need, both of which can have devastating consequences for the individuals involved.
Kudos to Florian Reider at Cleveland clinic for spear-heading a major effort to understand fibrosis in Crohn’s disease to develop novel therapeutics.
Ailsa Hart and Phil Tozer at St Mark’s with the Enigma consortium are making great headway with fistulising Crohn’s disease.
Both are long-term projects that need additional support to accelerate.
Treating patients holistically
This needs to start at diagnosis when there is an increased risk of mental health harm. A recent study showed that suicidal ideation and completed suicide were increased in the first year after diagnosis in Crohn’s disease.
Rates of anxiety and depression are increased in IBD.
But we have a severe lack of support in the clinic. Awareness is increasing amongst clinicians and patients but we must invest in psychological support services and frameworks to deliver responsive care.
Laurie Keefer has demonstrated that deploying a behavioural playbook in IBD - teaching patients individualised coping strategies to increase resilience WORKS. We must implement this at scale.
But holistic care is not just about mental health - it is about understanding the person that is living with IBD and the impact it has on their lives. It is about managing fatigue and sleep disruption, work and family planning, intimacy and dietary choices / restrictions.
Christine Norton is working hard on this with the IBD Boost programme that will tell us a huge amount about pain, incontinence and fatigue in IBD and provide evidence based intervention strategies.
So there is a big unmet need, but there is a lot of great work going on.
Frictionless monitoring strategies
We need to follow the diabetes community here.
People living with diabetes now can contiguously monitor their glucose level via an invisible patch on their arm with a smart mobile app and AI algorithms devivering insulin via small wearable pump.
Now the IBD problem is much harder than this. The closest we can get to blood glucose is faecal calprotectin. This requires poo. And that’s not trivial. Current point of care tests are cumbersome, unreliable and expensive.
We need innovative solutions for IBD to continuously monitor gut inflammation.
Prevention strategies
Ultimately the global IBD community wants away with IBD and that includes us. We want to cure those living with IBD and prevent it from developing in the first place.
To get there we need a huge co-ordinated global research effort. Tine Jess in Copenhagen is leading the way here with truly visionary leadership at the PREDICT center. This is bringing together efforts from across Europe and North America. We are working on this too. We really need to get into places where IBD is still in the emerging phases - parts of Asia, South America and in particular Africa.
What causes IBD? Can we detect early markers of pre-clinical IBD? The brilliant work by Jean-Fred Colombel in the US Veterans cohort, Ken Croitura leading the GEM Study (which we make a big contribution to in the UK), Joana Tores looking in pre-diagnosis teeth, and the Muconium Study are just a few examples producing meaningful data already.
We are about to see amazing data from the International IBD Genetics Consortium from large scale whole genome sequencing and a massive meta-GWAS analysis.
Understanding the genetic architecture of IBD drives mechanistic understand and reveals drug-able targets.
Once we have identified at risk individuals we need an intervention plan.
This list is not exhaustive. There will be important things I have glossed over. The unmet need in IBD is substantial and urgent. But we are aware and there is a lot of great work going on to understand it, develop solutions and implement them.
We need to ensure that there is diversity in clinical trials & equity of clinical care.
Let me know your comments. What would you add? Which do you see as the most urgent unmet need? Which problems have solutions within touching distance.
Let’s continue to work on this together and bring hope to our global IBD community.
Thank you for reading.







Excellent work as always. Absolutely agree priority needs are early diagnosis, right treatment first time, treatment of patients as a whole and proactive surveillance. (The chief medical officer's recent report on IBD stats in Scotland underlines more needs to be done for IBD patients too)
I would like to build on your comments re dietary influences on IBD. Absolutely research in this area is important. However societal (and sometimes scientific) presumptions on dietary influences and IBD can hugely undermine patients' burdens in overcoming societal misassumptions about disease cause, seriousness, treatment requirements and life impact. This happens more in IBD than other comparable disease. Research on diet and IBD needs to avoid the dangers of the correlation vs causation trap and take huge care in managing messaging to avoid "victim blaming" of patients with an awful disease which isn't their fault and the course of which is largely outwith their power to "control".
I also agree there needs to be much more joined up research and care on IBD "outside the bowel". I would like to see much more surveillance and understanding of correlating disease in eg eyes, skin, bones, other organs etc. For example, given my longstanding Crohn's diagnosis, delayed diagnosis of Anklosing Spondylitis and Uveitis could have been reduced if there was more focus and education on EIMs in IBD care and IBD correlating disease vulnerabilities. Neither patients nor primary care are educated on what to look out for and bowel symptoms are the narrow focus frequently in clinic. EIMs should be part of broader consistent IBD surveillance, targets, measurements and interdisciplinary care. The lack of IBD understanding more generally in primary care and lack of joined up specialist care worsens patient suffering, health outcomes and health economics.
I agree patients need much more support with the the psychological burden of disease. But I also think there is more work to be done on understanding and responding to the physiological impact of IBD and brain health in mental and neurological impact eg via gut-brain axis, inflammation effects on brain health etc. This understanding should constructively feed into treatment and support strategies in addition to "resiliency" support.
I am hugely supportive of improved disease surveillance measurements and patient and treatment stratification. However, I am also wary of risks of "healthcare by numbers". Narrow focus on calprotectin or "risk score" numbers can risk the importance of responding to the uniqueness of patient's experiences, needs and treatment responses.
Thank you for this article and power to you and your colleagues trying to identify and meet IBD patients' needs.