Stopping anti-TNF therapy in IBD: is it ever a good idea?
New data confirm high rates of relapse on stopping infliximab in Crohn's disease
Thank you for reading Atomic IBD. Welcome to all the new subscribers. If you have not yet subscribed please do so now to receive direct in your inbox.
What happens when you stop anti-TNF therapy in IBD?
In Crohn’s disease approximately 50% of patients will flare within a year.
These are the data from a rigorous randomised controlled study of over 100 patients from four Nordic countries published this week in NEJM Evidence. Recruited between 2013 and 2020, the patients were randomised to continue infliximab (n=59) or discontinue infliximab (n=56) after a median of 24 and 21 months of therapy respectively. The patients were in deep remission: median CDAI of 41, CRP 3mg/L and SES-CD of 0. The study was placebo controlled: those patients who discontinued infliximab went on to receive iv placebo infusion.
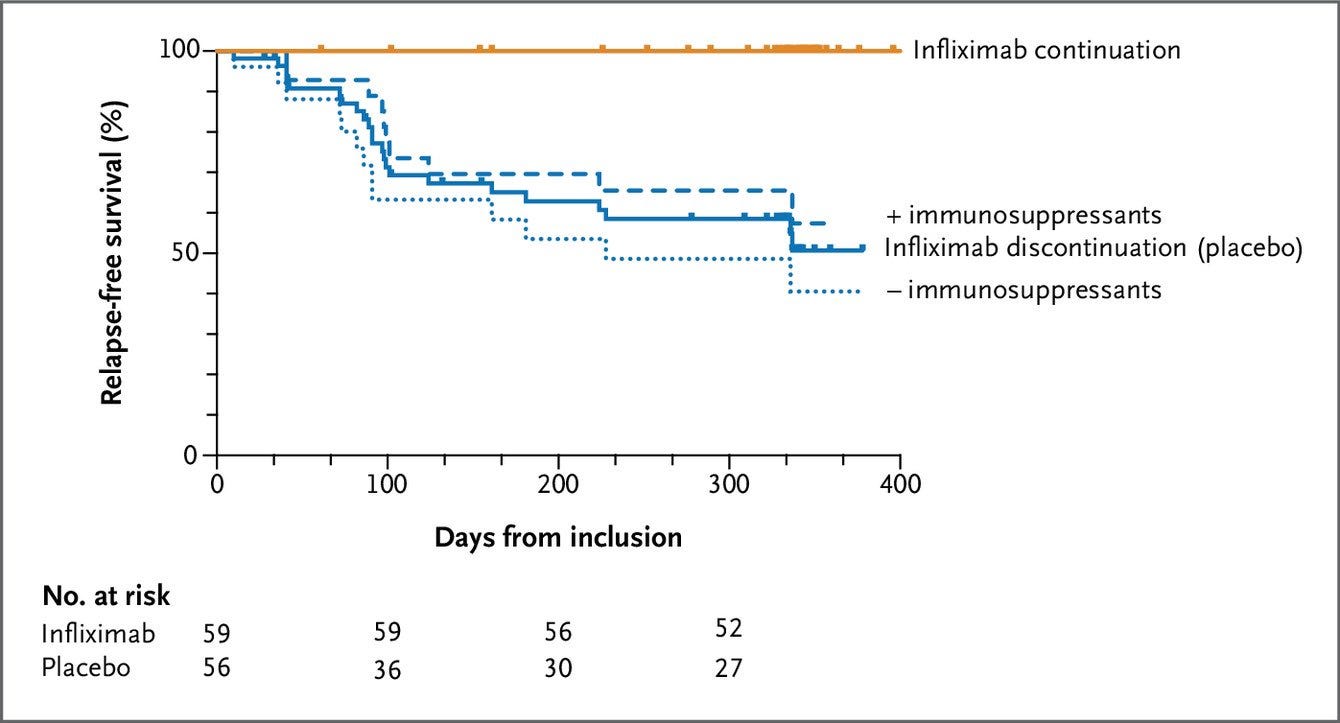
Discontinuation of infliximab resulted in disease relapse in 49% of patients versus zero in the continuation group. There was only minimal impact of thiopurine therapy as shown in this figure:
Can we predict who will flare on stopping anti-TNF therapy?
Unfortunately not. At least not in the study.
There were no predictors of disease flare when baseline characteristics - including demographics, disease location or behaviour, duration of disease or infliximab therapy, prior surgery or smoking status.
How do these data compare to those of the SPARE trial?
The data are similar and this is helpful for clinical practice.
The SPARE trial (presented at ECCO and DDW this year) randomised 211 patients on combination therapy (infliximab plus immunosuppressant) for at least 8 months to one of three arms: A continue therapy; B stop infliximab, continue immunosuppressant; C continue infliximab, stop immunosuppressant.
Relapse rates over two years in SPARE were 14%, 36% and 10% in the three arms.
The SPARE dataset provides additional findings:
out of 39 relapsers, 28 were retreated - of whom 25 (89%) obtained clinical remission
22 of 23 patients in arm B regained remission on restarting infliximab
the mean time in remission across two years was the same in each arm (see figure below)
younger age at onset and evidence of inflammation at baseline were associated with clinical relapse in all treatment groups
low 6-TGN predicted clinical relapse in patients stopping IFX
smoking predicted failure in patients stopping IFX
What can we conclude from these two important studies?
Stopping infliximab is associated with a high rate of relapse.
When patients are in deep remission, it is hard to predict who will relapse. However most patients will recapture remission on restarting therapy.
So what should we do in clinical practice?
Infliximab therapy is now very cost effective. Treatment continue / stop decisions should not be driven be cost.
For most patients the right path is continue with anti-TNF therapy and this is my usual recommendation in the clinic.
When patients are on combination therapy, I will sometimes look to withdraw the immunosuppressant and continue with infliximab monotherapy. The exception to this is with fistulising disease where I prefer to continue combo therapy.
How does this look like practically for a bionaive patient with a purely inflammatory phenotype starting combo therapy?
start infliximab standard iv induction and maintenance
start azathioprine at about 1.5mg/kg (usually 100-150mg once daily)
monitor infliximab drug levels and anti-drug antibodies
after 6-12 months, if no antibodies drop azathioprine dose down to 50mg
after approximately 24 months, if no antibodies stop azathioprine
note that this applies also to subcut infliximab but this may change as new data emerge
Despite all this, there will be some patients who would like to withdraw therapy for a number of possible reasons.
In this situation I would first check for deep remission: CRP, calprotectin and colonoscopy. I would then monitor bloods and calprotectin every two months for at least the first year and probably over two years.
At the first signs of a flare (eg rising calprotectin) I would restart therapy, not waiting for a full symptomatic flare to develop.
For comments, feedback and ideas please email interesting@atomicibd.com