Pros and Cons of different Advanced Therapies as first-line agents in Crohn's disease
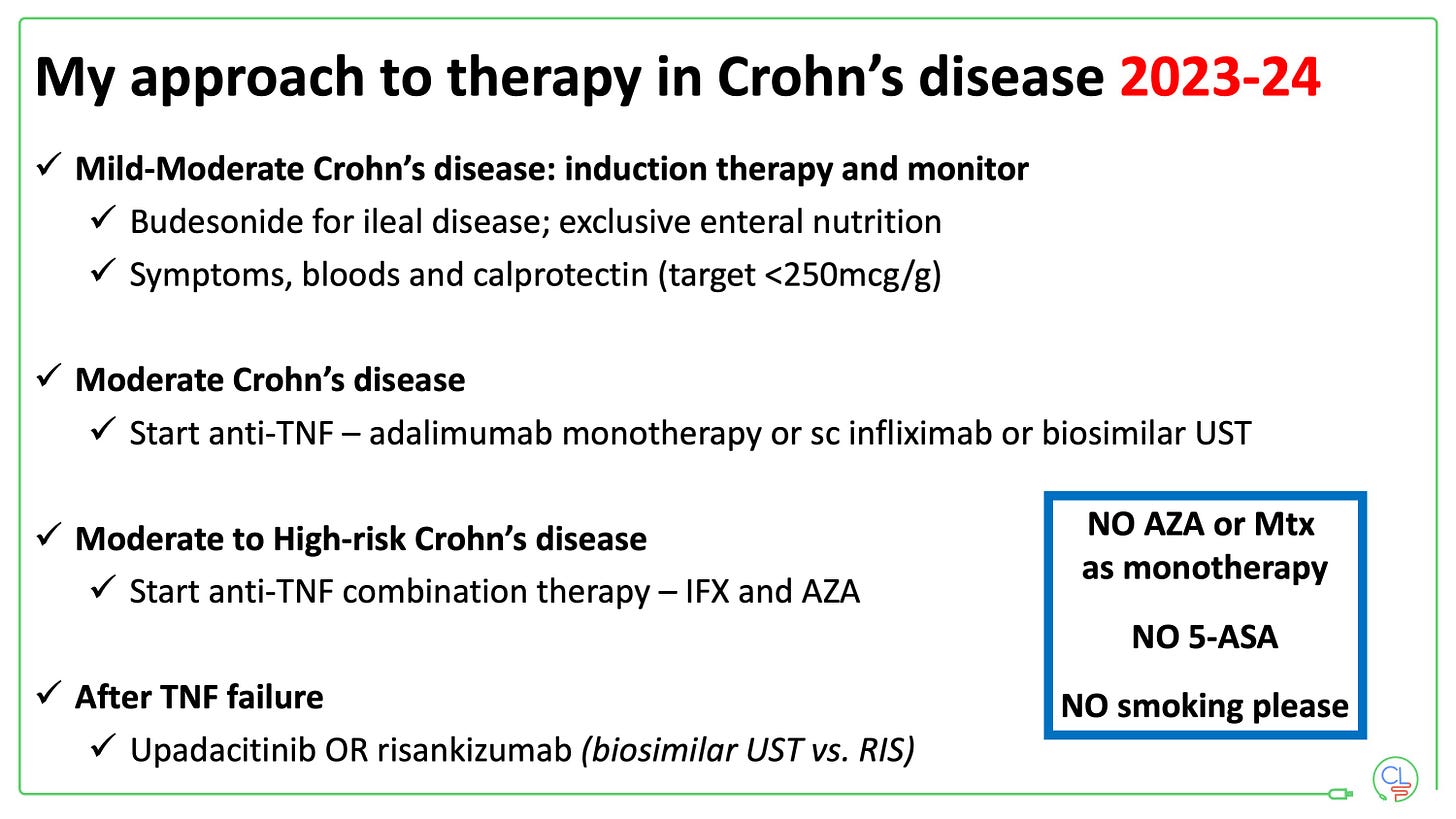
Early effective therapy in Crohn’s disease is the best way to improve outcomes for patients.
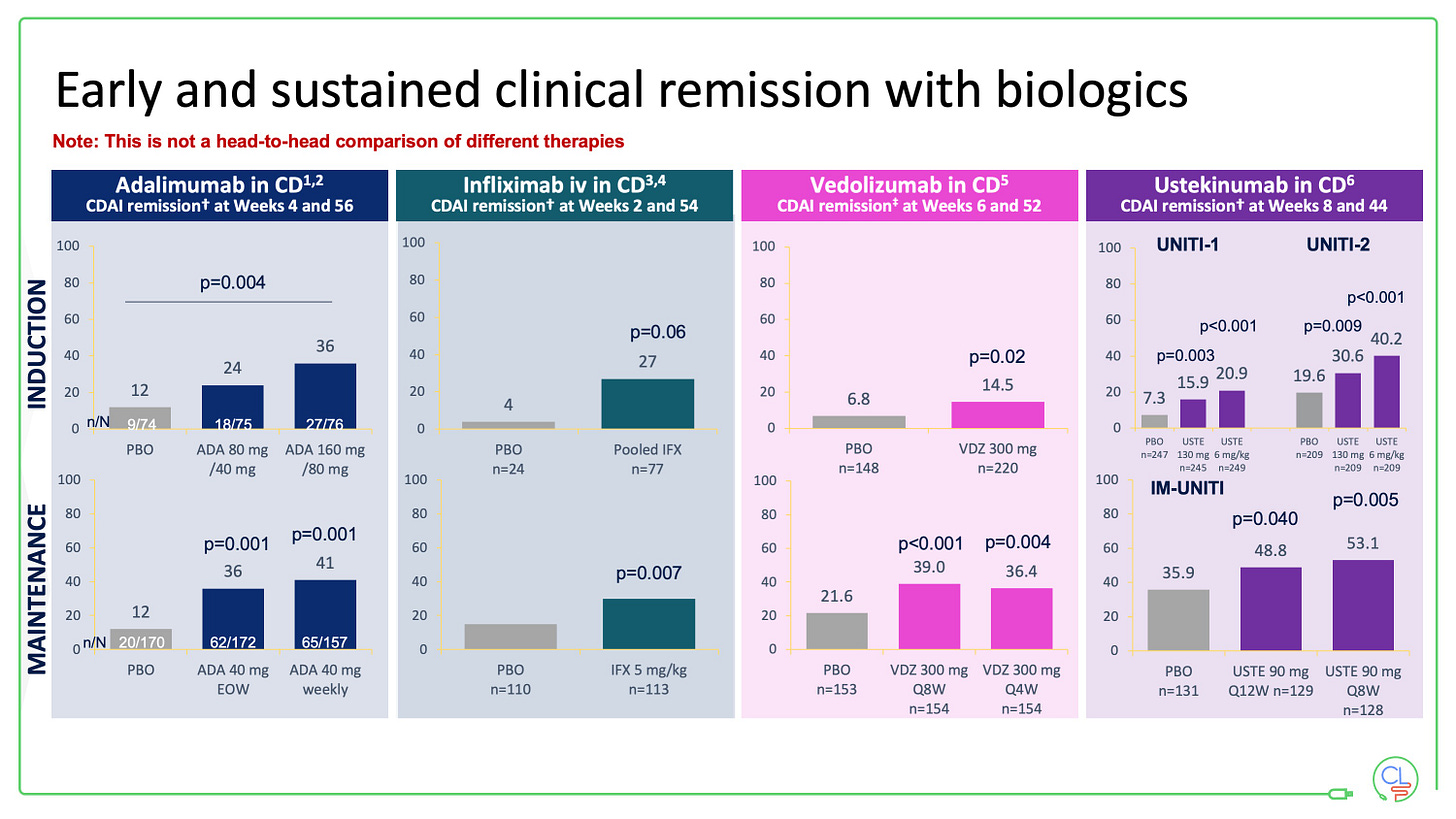
Multiple lines of evidence now support this using biologics - notably with anti-TNF therapy, but not with conventional immunomodulators.
The best chance of success for all IBD patients is with their first advanced therapy.
With multiple effective agents now approved for use in Crohn’s disease, what are the pros and cons of each as first-line agents?
Infliximab (iv) plus azathioprine
Pros: highly effective, multiple lines of data, cost-effective, combo therapy best way to minimise immunogenicity, widely available
Clear evidence of efficacy - SONIC (2010) demonstrates combo therapy better than mono therapy with infliximab which is better than mono therapy with azathioprine
Cons: slight increased risk of infection, early monitoring, infusion facility required, long term durability poor even with comb
Infliximab (subcutaneous)
Pros: highly effective, favourable pharmacokinetics vs iv IFX
Cons: cost (more expensive than iv IFX) and unanswered questions:
Is monotherapy with subuct as effective as combo?
What are secondary loss of response rates with monotherapy after 1 year?
Is persistence better than with iv infliximab?
Adalimumab (mono or combo)
Pros: cost effective (cheapest of all advanced therapies), reduced immunogenicity compared with infliximab
Cons: likely less effective than infliximab (? delta), durability still not great (esp when used a monotherapy)
Ustekinumab
Pros: as effective as adalimumab monotherapy (SEAVUE) when used as first-line agent; long-term persistence likely better; safety profile more favourable than anti-TNF; biosimilars available in 2024-25
Cons: currently expensive; limited data on first-line use in Crohn’s disease; less effective for fistulas than anti-TNF
Vedolizumab
Pros: excellent safety profile; most effective in early, milder disease,
Cons: expensive; slow onset of action; less effective in moderate-severe disease and fistulas;
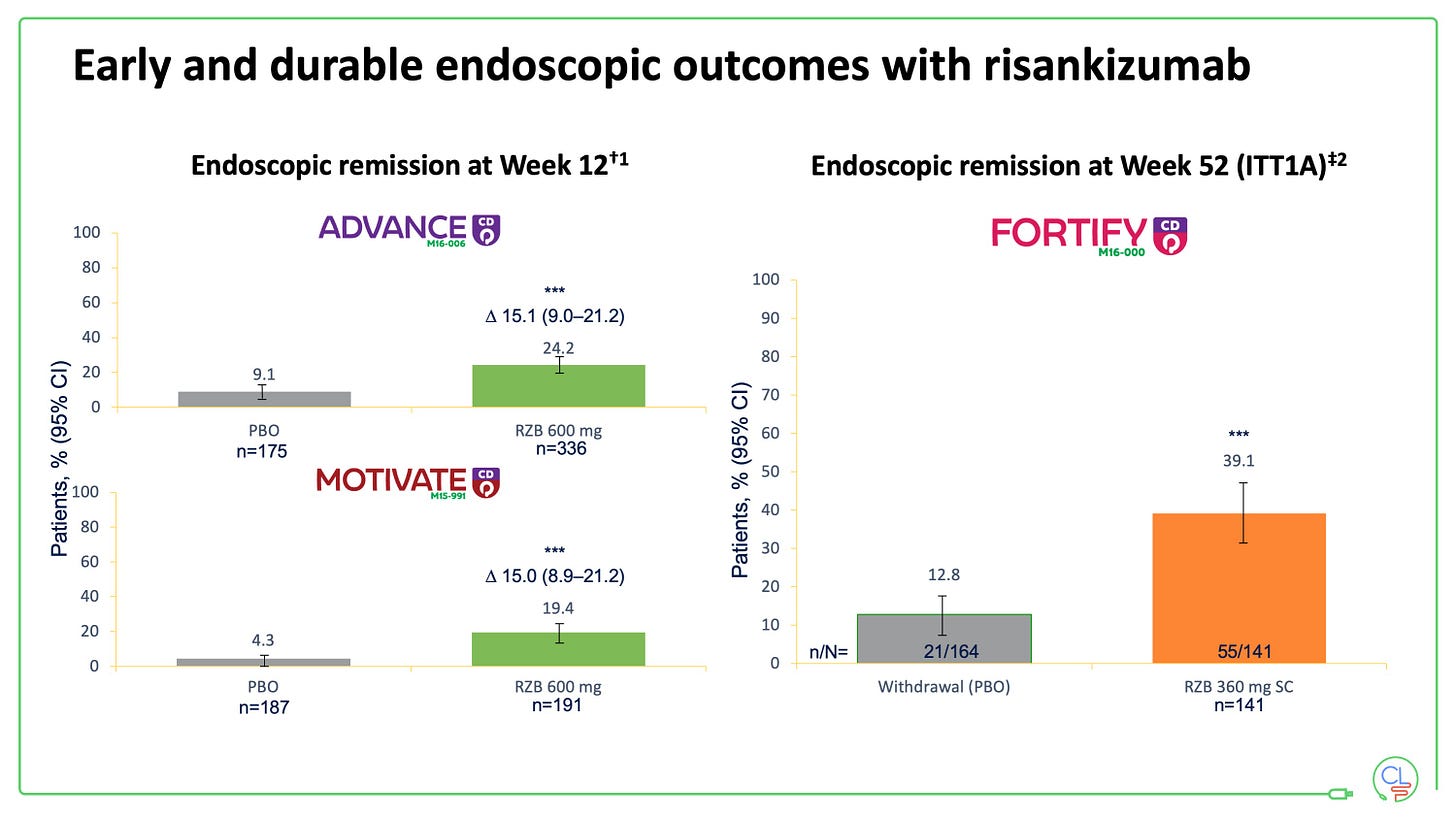
Risankizumab
Pros: highly effective especially as first-line agent; excellent safety profile; long-term persistence expected to be very good
Cons: expensive; can take 24+ weeks to reach maximum effectiveness; requires infusion suite for 3x induction doses and on-body device for maintenance
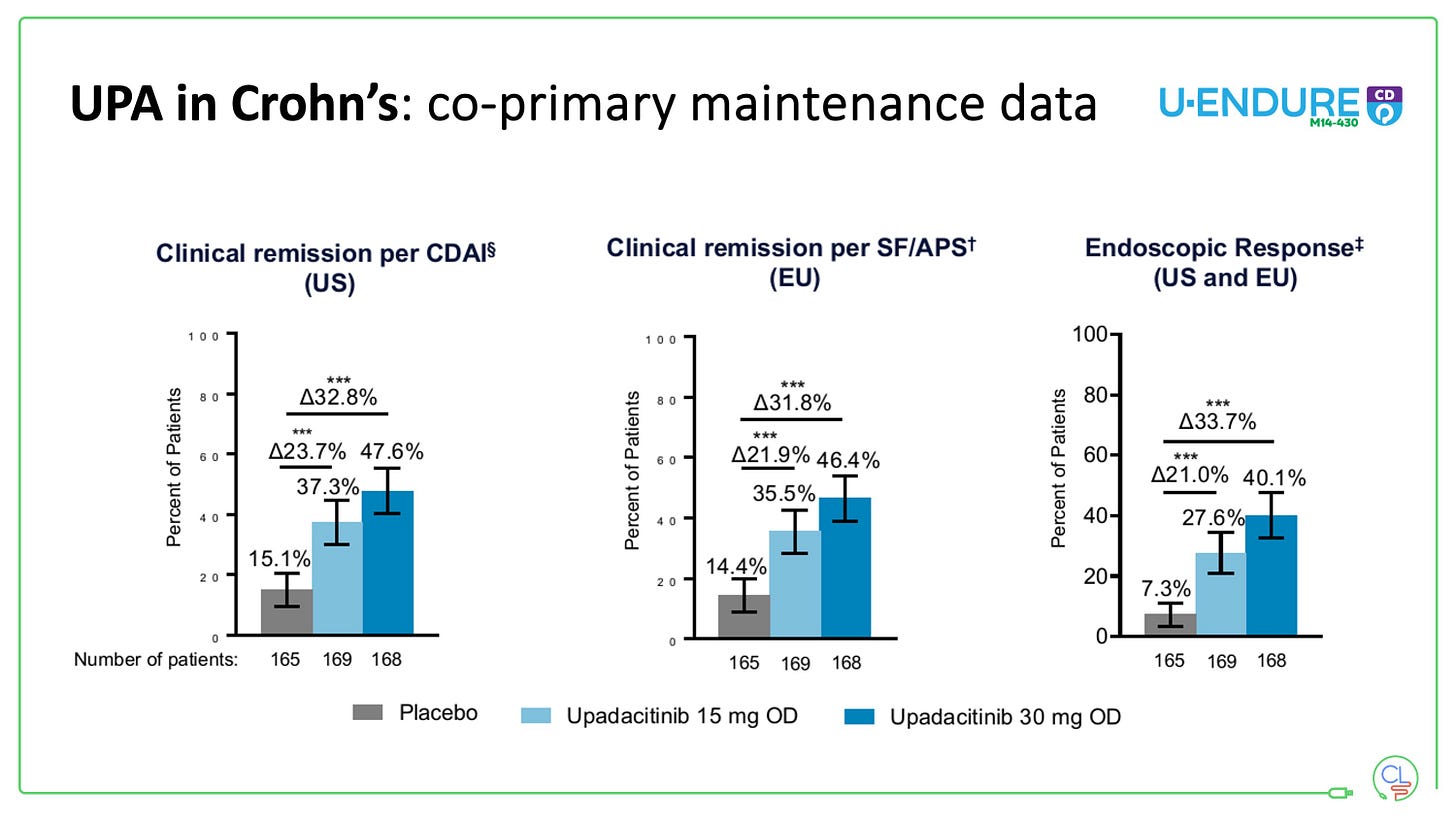
Upadacitinib
Pros: highly effective; rapid onset of action; oral, once per day
Cons: limited data on first-line use; first-line use only approved in certain regions (including Scotland); FDA & EMA have warnings on all JAKi;





I read an excellent article about drug therapy for Crohn's disease. However, it seems that the disease has a cure only for patients who are fortunate enough to be in a particular country while being unlucky for others. As a CD patient myself, I feel that the article speaks only to privileged patients and not all patients. It is disheartening to know that there is a treatment that could relieve the pain and suffering, but we do not have access to it. I know from experience that a biological treatment can put me into remission, but I have not been able to receive it since 2019.