IBD at the start of 2023: part 1 - exploring gut inflammation research
12 papers on gut inflammation from the past 12 months.
I am an optimist who believes hope to be a powerful medicine.
The world of IBD research is moving fast and in some very exciting directions. Many new molecules are entering clinical practice, targeting multiple different mechanisms. As a clinician I can already see the impact these new therapies can have on patient lives. And also the limitations - none of our new drugs are a panacea for IBD.
The breadth and depth of outstanding basic and translational research on gut inflammation has been incredible over the past 12 months. As a scientist it is fascinating to follow and assimilate these new data. Much of the new data has challenged existing paradigms demonstrating the power of robust experimentation and application of new methodologies.
These data are the fuel for new hypothesis generation and clinical application.
Timescales for true translation from bench to bedside will stretch over very many years if we are not careful. Every effort should be made to prioritise, fund and deliver on translational clinical trials that take turn the best ideas to direct clinical utility. But we should also be patient and not short-cut rigorous testing in the pursuit of speed.
Who decides which ideas are the best, which trials the most important, which data most impactful? We should not be too dogmatic about what gets done where, and by whom. Instead let us ensure that data and ideas are free to flourish in the world.
The power of ideas coupled with distributed digital media is central to my mission here with Atomic IBD. To share, assimilate and reflect on new data. And in so doing to provide hope.
12 papers on gut inflammation from the last 12 months
These are the scientific papers that had the biggest impact on me this year.
Heavily focused on diet and the microbiome
High quality papers from the 3 apex journals: Nature, Science and Cell.
These are the papers that make me most excited for the future.

1. Klebsiella pneumonia increased in IBD and killed by a cocktail of phages
Phage cocktail shown to treat colitis in mouse models and to alter microbiome in healthy individuals
An exciting window into future microbiome therapeutics
https://www.cell.com/cell/fulltext/S0092-8674(22)00850-9
The figure below is from an excellent commentary in Nature by Alice Pertocchi and Fiona Powrie (A Viral Cocktail Calms Inflammation).
2. Environmental toxins and intestinal inflammation
Specifically: propyzamide - a herbicide
This was identified through an amazing series of experiments - zebrafish / artificial intelligence screen and beautiful mouse models
https://www.nature.com/articles/s41586-022-05308-6
3. Fermented foods versus high fibre diet in man
Surprising results: fermented foods have greater positive impact on microbiome diversity and reduced inflammatory signalling
Begging for a trial of kefir, kimchi, kombucha and other fermented foods in IBD
https://www.cell.com/cell/fulltext/S0092-8674(21)00754-6
4. RCT on the effect of non-nutritive sweeteners in man
Demonstrating the impact of sucralose and saccharin on the gut microbiome (causally linked to glycaemic responses)
What is the impact on gut inflammation models?
https://www.cell.com/cell/fulltext/S0092-8674(22)00919-9
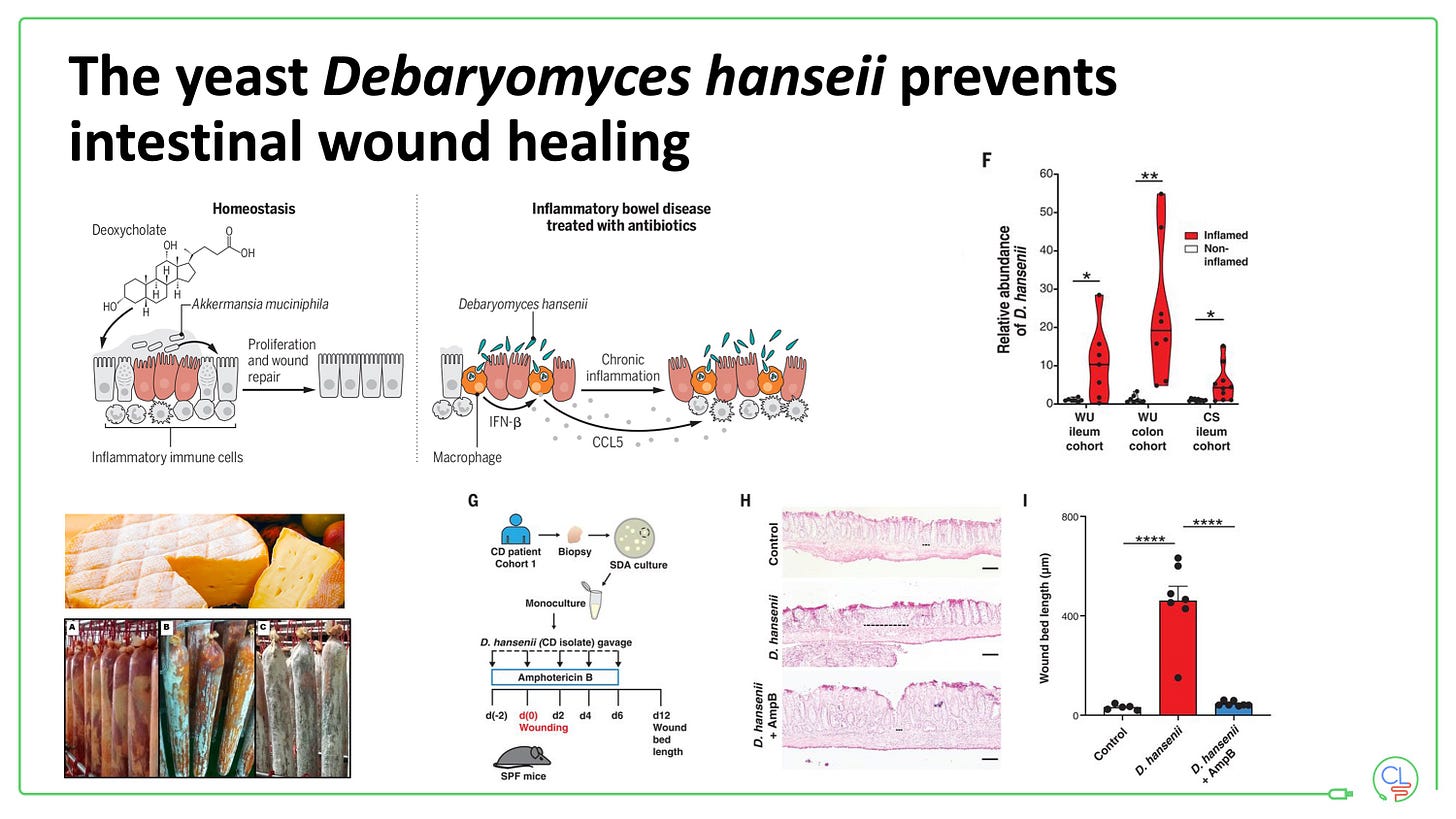
5. Debaryomyces hanseii and Crohn's disease
A yeast - found in cheese and cured meat rinds - is found in high concentrated in Crohn's disease ulcers
In models this yeast prevents ulcer healing and thus perpetuates intestinal inflammation
https://www.science.org/doi/10.1126/science.abd0919
6. Candida albicans and colitis
Certain strains are expanded in the colonic mucosa of patients with UC
Promote inflammation in mouse models of colitis via production of candidalysin
https://www.nature.com/articles/s41586-022-04502-w
7. Ultra-processed foods and the risk of IBD
Appear to increase risk of Crohn's disease, although difficult to fully control for confounders in these population based cohorts
Similar data recently from the PURE cohort and UK Biobank
https://www.bmj.com/content/374/bmj.n1554.long
8. PUFAs acts as fuel for intestinal inflammation in Crohn's disease
A predominantly small bowel effect, restricted by epithelial GPX4
Does not initiate disease, but may be one driver of chronicity.
https://www.gastrojournal.org/article/S0016-5085(22)00012-9/fulltext
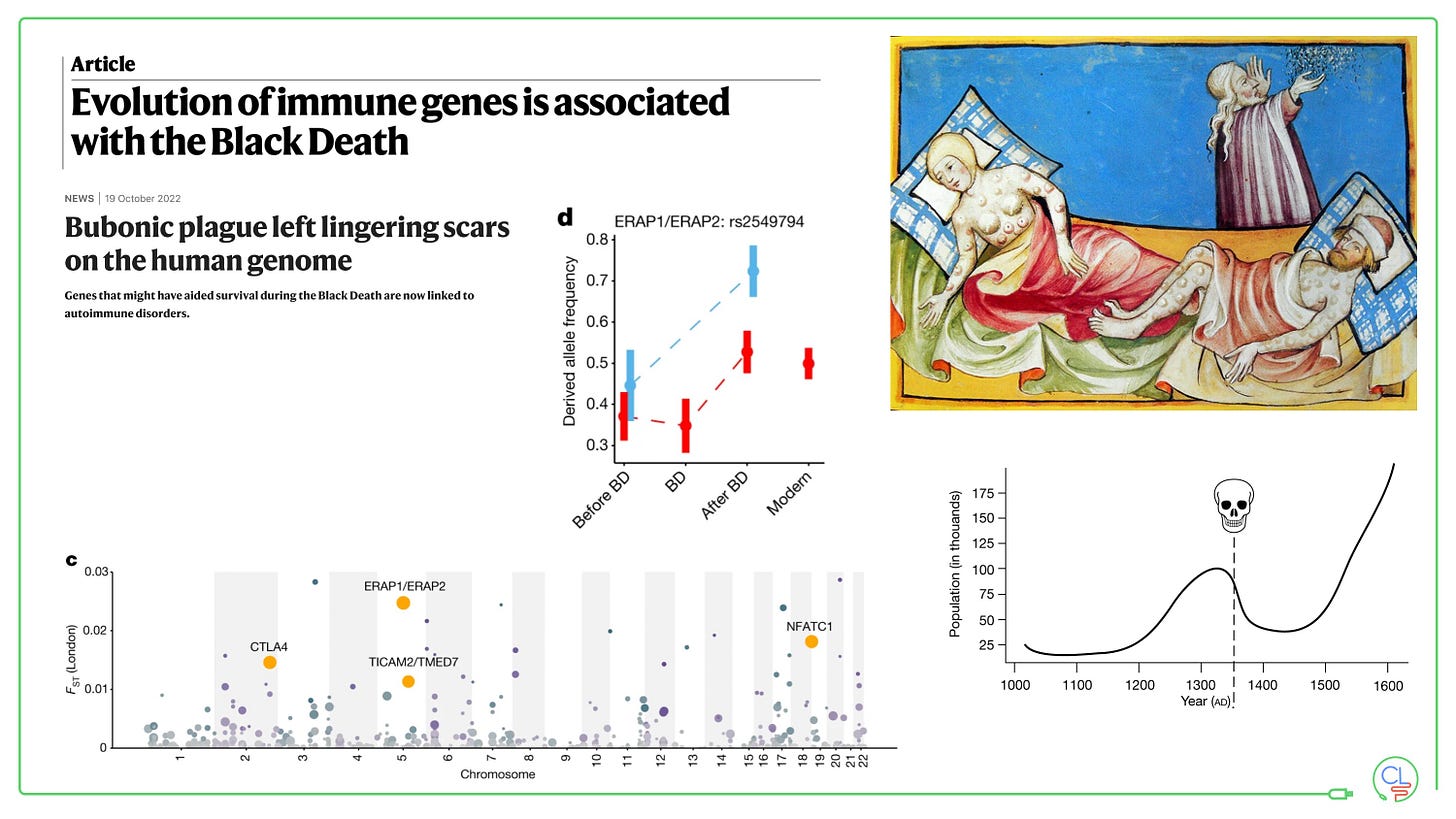
9. Effect of the black death on immune genes
Four genes show significant positive selection after the black death, including ERAP2 - a Crohn's disease gene.
A mutation that protected against plague in 1300's increases risk of Crohn's disease in 21st Century.
https://www.nature.com/articles/s41586-022-05349-x
10. Genotoxic small molecules produced by the microbiome of patients with IBD seem to drive intestinal tumorigenesis
Indolimines produced by gram negative bacteria - Morganella morganii
https://www.science.org/doi/10.1126/science.abm3233
11. Human gut bacteria produce ΤΗ17-modulating bile acid metabolites
3-oxoLCA and isoLCA inhibit TH17 cell differentiation
Their levels were reduced in patients with IBD and inversely correlated with expression of Th17 associated genes
https://www.nature.com/articles/s41586-022-04480-z
12. Innate lymphoid cells (ILC3's) control the fate of inflammatory versus tolerogenic T cells in response to specific microbiota in the gut
Interactions between ILC3s and RORγt+ Treg cells are impaired in IBD - strategies to fix this may be critical
https://www.nature.com/articles/s41586-022-05141-x
Coming in the next Atomic IBD …
In part 2, I will explore the exciting new therapies for IBD. I will highlight the key publications from last year and preview the developments anticipated in 2023.






Hi Charlie, could you address the pediatric crowds for the upcoming part 2 as well?