Six key parallels and lessons that IBD can draw from today's cardiovascular-disease editorial in the Lancet
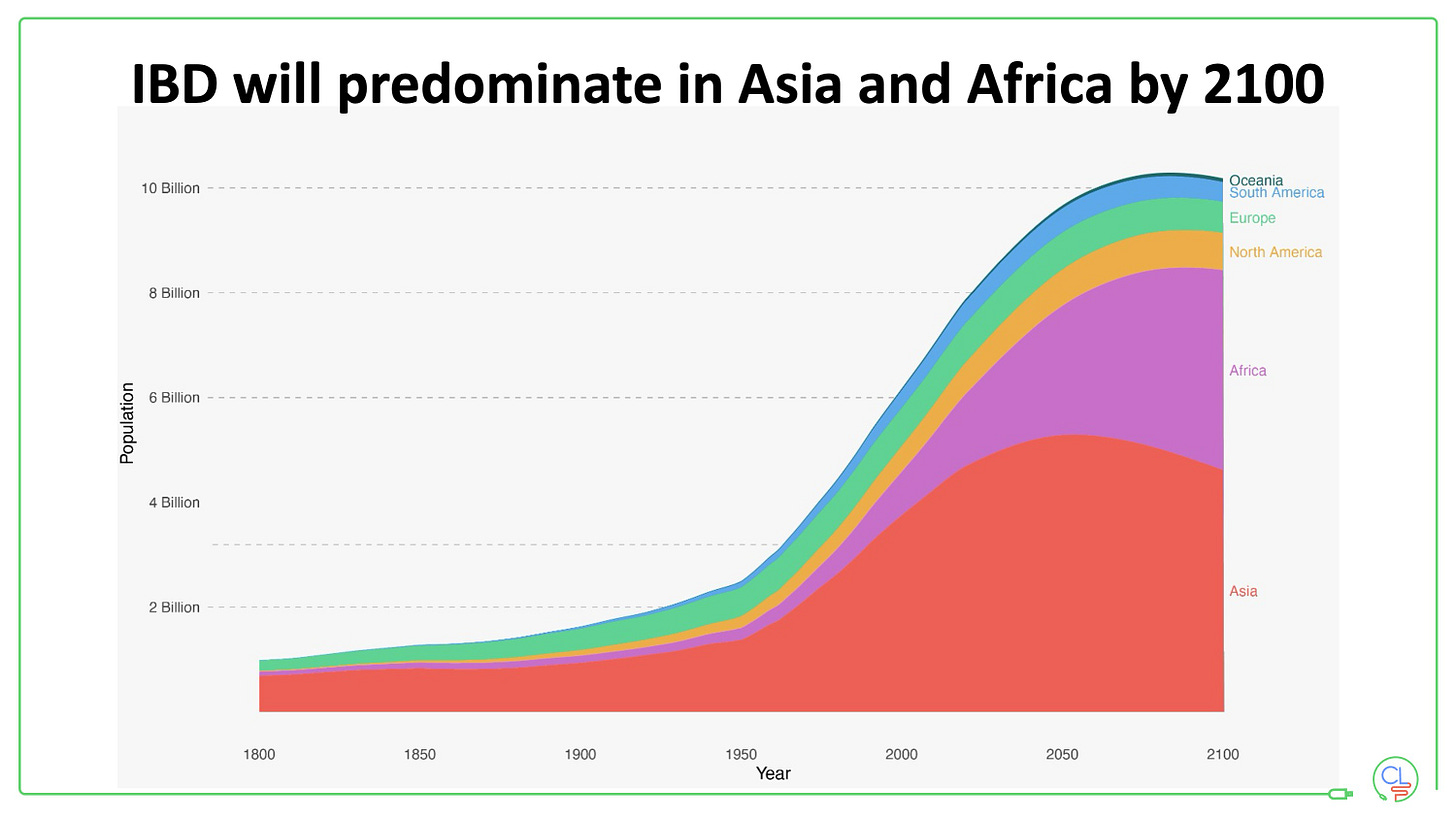
The burden is shifting toward low- and middle-income countries (LMICs).
More than three-quarters of all cardiovascular deaths now occur in LMICs, forcing cardiology to rethink delivery models beyond high-income settings.
IBD is on the same trajectory, with incidence climbing fastest in newly industrialising regions, so LMIC-ready care pathways must be built early.
The figure shows global population growth by region this century.
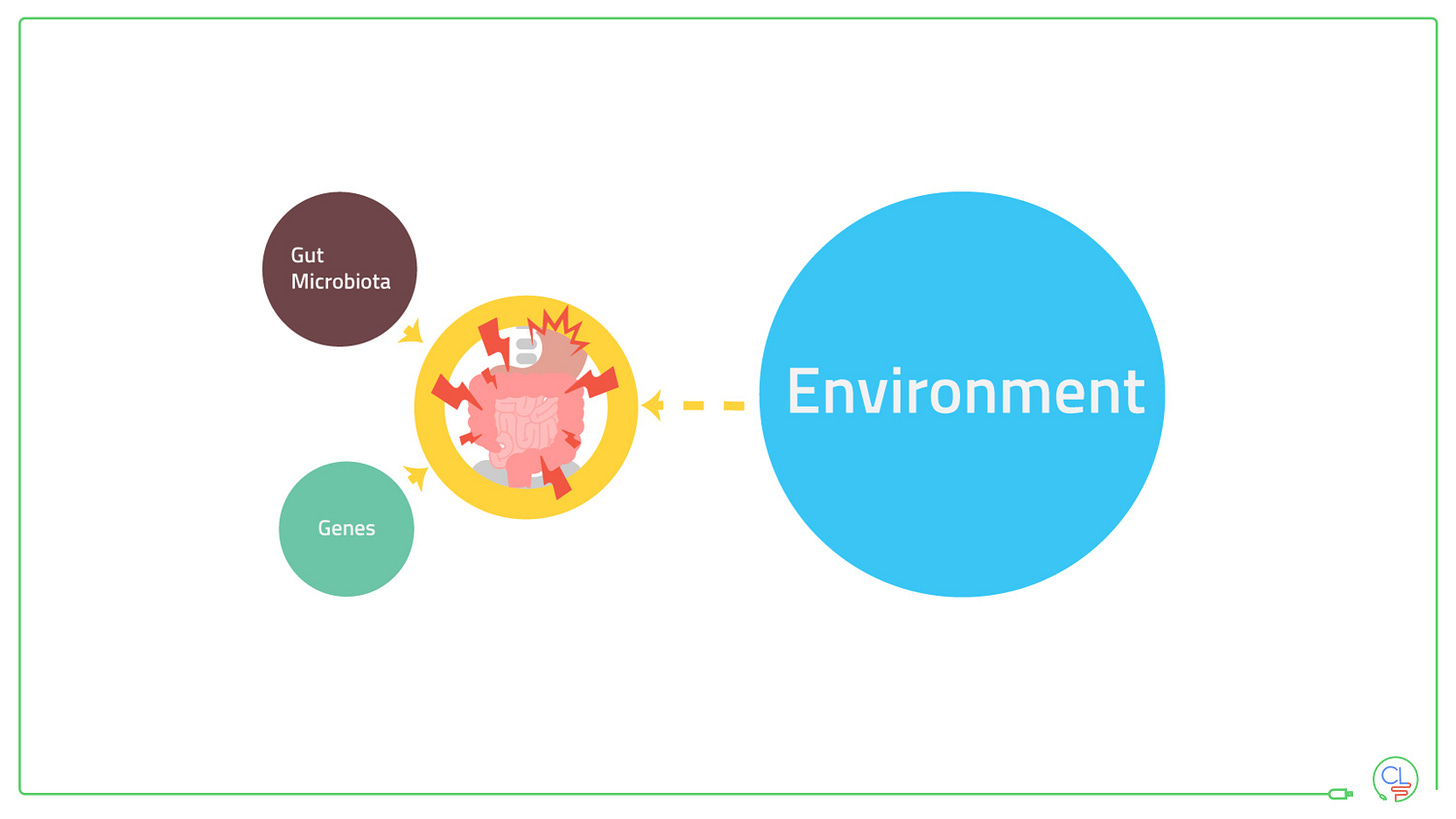
Mechanistic blind spots slow progress.
Heart-failure with preserved ejection fraction and several other CVD phenotypes remain poorly understood at the molecular level, limiting target discovery.
IBD likewise lacks robust biomarkers that can align patients with its expanding menu of biologics and small molecules, underscoring the need for deep, multi-omics research that includes diverse populations.
Innovation means little without implementation.
Breakthrough drugs and devices exist, yet statins are stocked in only ~5 % of public clinics in many LMICs and advanced cardiac procedures are virtually absent outside tertiary centres.
IBD faces a parallel gap: biologics, JAK/S1P inhibitors and even routine colonoscopy remain inaccessible for most patients in low-resource settings, so cost-contained, scalable delivery models must be planned alongside every new therapy.
Policy-tackled, modifiable exposures matter as much as high-tech fixes.
Tobacco control, salt reduction and active-transport urban design are now core CVD counter-measures.
Analogous levers—dietary-fibre promotion, restrictions on emulsifiers, antibiotic stewardship and smoke-free policies—could blunt the coming IBD surge if written into public-health strategies soon.
Low-tech, community and digital tools stretch specialist reach.
Simple SMS reminders and community health-worker home visits have improved blood-pressure control but remain under-scaled in cardiology.
Comparable text-based flare alerts, stool-calprotectin pick-up points and nurse-led support could extend IBD care into primary settings.
Equity has to be built in from the bench.
The editorial calls for research that “spans the full spectrum from bench to community,” stressing implementation equity so innovations actually reach the poorest populations.
Global IBD consortia should therefore embed LMIC sites in trials, share data openly and pre-plan technology transfer for any diagnostic or drug that proves effective.