First impressions of ECCO 2024 - starting with early effective therapy in Crohn's disease
Putting PROFILE into context for the global IBD community
Stockholm was cold, dark and moody these February days.
ECCO in contrast was vibrant, buzzing and alive with the best scientific programme in recent memory. I’ve come back more invigorated, with more to think over and with boundless optimism for the IBD community.
This year we saw pivotal trials with immediate practice changing implications, effective new molecules and treatments strategies, and a depth of quality translational science that I don’t remember from previous years.
In fact I’m convinced that the meeting is now too short to do justice to a global organisation attracting this volume of quality research.
I would scrap all the pre-ECCO activities and extend the full meeting by a full day.
With far too much new data to summarise in one article, you can look forward to several updates from Atomic IBD over the next days and weeks.
We are starting with my thoughts on the PROFILE study, the clinical aspects, the failure of the biomarker and the implications for our global IBD community.
Early, effective therapy in Crohn’s disease
The landmark PROFILE study finally puts to rest any doubt about the best treatment strategy for Crohn’s disease.
Treat early, very early, and use effective therapy from the start.
PROFILE clearly demonstrates the superiority of a top-down approach over accelerated step-up in newly diagnosed Crohn’s disease.
Infliximab and azathioprine, when initiated just 2 weeks after diagnosis, is far superior to waiting a few months before starting azathioprine, and longer still before starting an anti-TNF.
At 1 year the outcomes in the top-down arm vs step-up arms were:
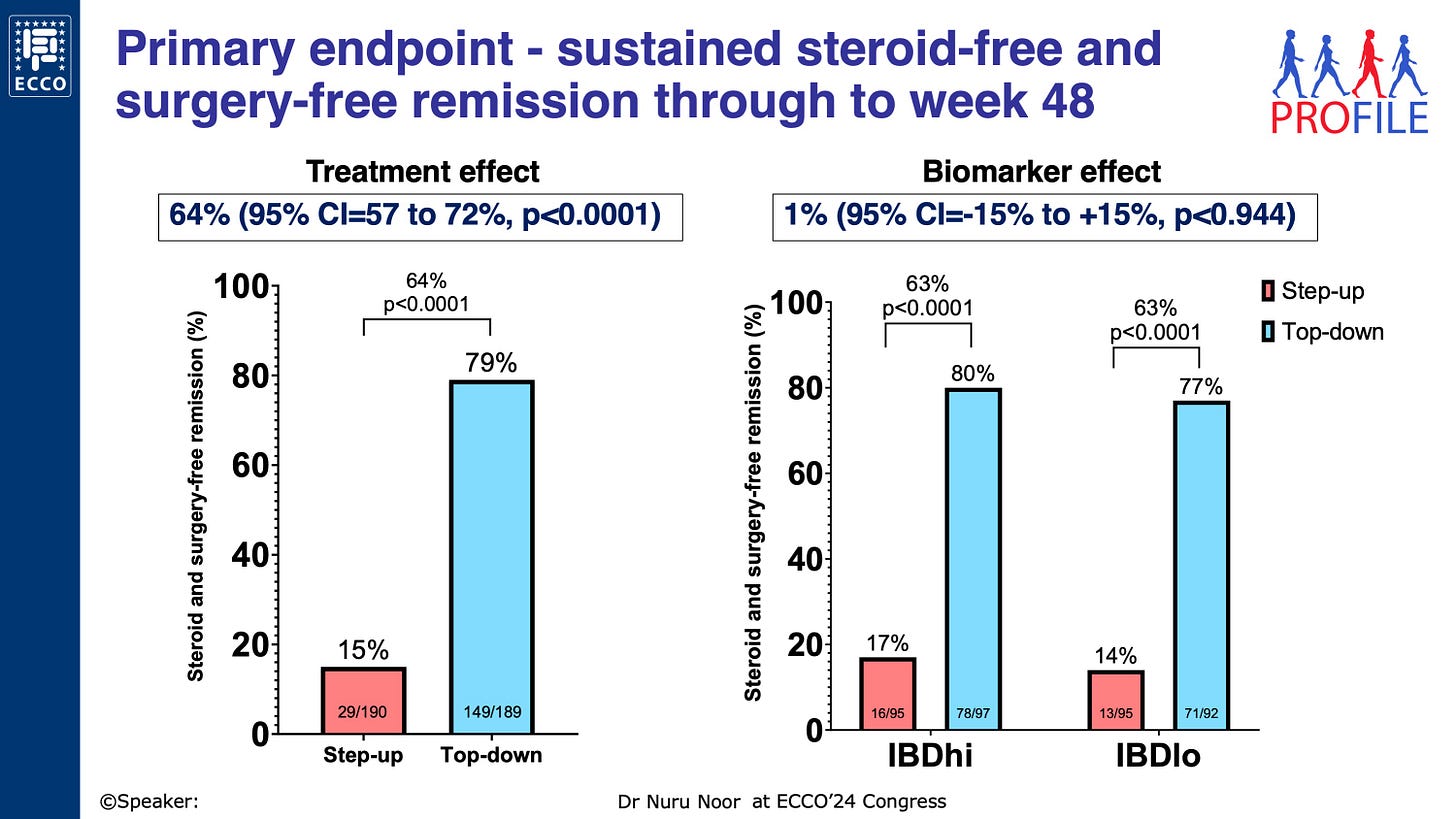
79% vs 15% steroid and surgery free clinical remission
67% vs 44% endoscopic remission
1 vs 10 urgent abdominal surgeries
30 vs 225 Crohn’s disease flares
3 vs 8 severe infections
Time to first and second flares are shown in both groups in panels A and C in the figure below. This visualisation allows you see the events that trigger step-up to azathioprine (panel A) and infliximab (panel C) in the lower orange line.
So… does everyone need top-down therapy with IFX & AZA?
In my opinion, the answer is a clear no.
Many patients will likely be fine with any effective therapy early on (infliximab plus azathioprine, or adalimumab monotherapy, or ustekinumab or risankizumab or vedolizumab), so long as it is started early (at diagnosis)
Some patients only need a course of steroids or equivalent (eg enteral feeding).
If these patients do not normalise FC/CRP, then start effective therapy (still within 3m of diagnosis or as soon as possible)
But the majority of people with newly diagnosed Crohn’s disease should start effective therapy early (at diagnosis) and PROFILE shows just how effective this is after one year.
But didn’t we already have a step-up vs top-down study in Crohn’s disease?
Yes, published way back in 2008 by Geert D’Haens (in the Lancet here).
The original step-up versus top-down study also demonstrated the superiority of early combined immunsosupression when compared with step-up therapy.
Note that in this study the combination of IFX and AZA was for induction only; after which the IFX was episodic as required. It turns out this is a terrible idea unless you really want to induce anti-drug antibodies.
In her plenary talk, Severine further compared the two studies:
median time from diagnosis to treatment was 14 (2008) and 12 days (2024)
proportion with L1 disease 21% (2008) vs 33% (2024)
smoking rates were 43% (2008) and 24% (2024)
Why then did we not adopt top-down therapy in 2008?
There were likely three major factors.
the lack of IFX maintenance therapy in the D’Haens study;
the guidelines did not update;
most importantly COST.
SONIC (2010) then showed us that IFX was better than AZA and IFX plus AZA best of all. After that, we said:
“if infliximab was the same price as azathioprine we’d use it all the time”
And when that time came in 2015, many of us followed this approach (this figure shows our data on time to first biologic in Edinburgh over 4 distinct eras).
But most people did not and the guidelines did not update.
Now the bad news
The PROFILE biomarker showed no benefit at al - zilch, nada, not a bit.
And yes, for those of us who believe passionately in a future of personalised and precision medicine for IBD, this stings a lot.
The great hope was that we could stratify patients by the transcriptomic signature in blood and use that to determine who you treat early.
Look at the right hand panel in the top figure - there is no difference in the primary endpoint in the biomarker Hi and the biomarker Lo groups;
And panels B and D in the second figure - time to first and second flare is identical in both biomarker groups.
Remember that the PROFILE study only happened because the original CD8 T cell transcriptomic biomarker had shown such promise in independent prospective cohorts. The key paper was published in 2011 (Gene expression profiling of CD8+ T cells predicts prognosis in patients with Crohn disease and ulcerative colitis).
So it is back to the drawing board for precision biomarkers in IBD. I’ll write more later about the ongoing efforts in this field and why I remain very optimistic.
What does PROFILE mean to the global IBD community?
Whilst many of us have been practising a top-down strategy for several years already, this is absolutely not the current standard of care.
The overwhelming majority of newly diagnosed patients with Crohn’s disease across the world are marinaded in steroids and forced to endure months or even years of sub-optimal therapy with thiopurines and on-going active inflammation.
This equates to a very substantial degree of morbidity.
For some it is access to drug therapy, and this remains a barrier. But for many it has been either skepticism about early biologics or overly prohibitive guidelines.
PROFILE should now change this.
And then any harm done by combination therapy in a tiny minority (remember the safety profile was better in the top-down arm) will be offset by removing the enormous harm being done by under-treatment of the majority.
You can already read the full PROFILE paper online here A biomarker-stratified comparison of top-down versus accelerated step-up treatment strategies for patients with newly diagnosed Crohn's disease (PROFILE): a multicentre, open-label randomised controlled trial.






What does PROFILE say about treatment for newly diagnosed crohns patients who have only received their diagnosis from the histology of a right hemicolectomy?
Thanks Charlie, any thoughts as to why the proportion of L1 disease has increased since 2008?