San Diego, 4 May 2025
Below are the six Twitter threads I posted live from Digestive Disease Week today, gathered here in one place for the Atomic IBD community. They appear exactly as they were published—no edits, no extra commentary.
Is the gut microbiota an actor in IBD pathogenesis?
Complete masterclass by Harry Sokol @h_sokol #DDW2025
Is the gut microbiota an actor in IBD pathogenesis?
YES, and translation to the clinic is on the wayComplete masterclass by
@h_sokol #DDW2025Modify gut microbiota impacts disease severity
• In mice models
• In humans (FMT)Faecal microbiota from patients with IBD exacerbate colitis in mice
Altered gut microbiota in IBD – bacteria and fungi and viruses – with decreased diversity and change in composition
The alterations in the gut microbiome precede development of CD by several years and occur in the absence of inflammation in the gastrointestinal tract (GEM study)
Therapeutic strategy –
Hit the bad guys:
Antibiotics _ risk of antibiotic resistance and toxicity
Phages _ advantages as more targetedBoost the good guys:
FMT – has some effect but impossible to standardise; huge complexity underlying the FMT effect
Need for more controlled and scalable treatments than FMTConcept of bacterial consortia
Members working together (simplified microbiome)
Sum of individuality (each having a specific effect)Bacteria that boost Tregs
17 strains from human gut – colonise GF mice – induce Tregs and protective effects
VEDANTA Biosciences now moving into the clinicExtreme bacterial consort – one single well-chosen bacteria
F. prausnitzii – decreased in microbiome of IBD; member of phylogenetic core; dominant species > 5 % of the human microbiomePhase 1/2a clinical trial in CD completed
EXELIOM biosciences – phase 2 study in post-op CD initiatedPost-biotics – molecules produced by the microbes with a biological effect
Eg SCFAs (Butyrate), tryptophan metabolitesConsideration to position microbiome-based drug in the treatment strategy
Most of microbiome-based strategies are not “brutal immunosuppressants”Is treating the flare the most challenging problem in Crohn’s disease?
NO – most of the time we can find a way to calm down inflammation
It is ok to use very powerful short-term immunosuppressionIMPACT-Crohn study – target both immune system and microbiome after achieving remission
Steroids to induce clinical remission (n = 8 with FMT and n = 9 with sham = pilot study) randomised to single FMT or sham FMT via colonoscopy
Follow-up study ongoing in CD as a relay after TNF withdrawalConclusions:
• Need for a paradigm shift regarding drug positioning
• In IBD context: distinguish treatment for induction and maintenance
• Keep in mind the nature of microbiome-based drugs = not “brutal” immunosuppressant
IBD Treatment Paradigms: past, present and future
by David Rubin @IBDMD #DDW2025
What is a treatment paradigm?
Established approaches and strategies used in medical care for specific diseases or conditions
Involves a combination of therapies (surgery, medications and other interventions like diet) to achieve optimal patient outcomesTraditional strategies that define treatment paradigms
• Sequential monotherapy
• Step up and combo therapy
• Targeted therapy
• Precision medicine
• Combination therapies
• ImmunotherapiesOPTIMAL PATIENT OUTCOMES IN IBD
Unrestricted high QoL
Sustained control of bowel inflammation
Unencumbered personal and professional functioning
Healthcare that is affordable
General forces and factors in the development of treatments for IBD
· We do not know the cause and do not have medical cures
· Recognition of the chronic nature of IBD and phases of managements
· Development of outcomes of interest: short-term and long-term
· Evidence-based medicine
· Development of regulatory pathways for drug approval
· Advancements in technology
· Market forces and competitionTreatment paradigms in IBD
Desperation
Sequential monotherapy
Step-up
Top-down
Treat to target
Combination therapies
Biomarker driven
Cellular immunotherapyThe era of desperation in IBD marked by a multitude of evidence-free therapies: including horse serum, artificial fever therapy, hot water enemas, tincture of iodine and intracolonic insufflation of oxygen
Early surgical approaches in IBD: presumed “parasympathetic overactivity” or central nervous system causation; thymectomy in UC and bypassed loops of bowel in CD
Early approaches to diet in IBD: including elimination of raw fruits and vegetables, hyperalimentation with protein hydrolysates, bowel rest, fish oil
SEQUENTIAL MONOTHERAPY, STEP UP
Fail first, complications, delayed treatmentsTreatment breakthroughs
Prontosil rubrum (1935, the source of sulfanilamide)
Antibiotics
Sulfasalazine (Professor Nanna Svartz, Karolinska)
Steroids
Mesalamine
Infliximab – taught us a lot about disease biologyEarly step-up strategies –
Pyramids – staircases and lots of failuresTop-down – early effective therapy
This is the superior strategy for patients with Crohn’s diseaseProliferation of new therapies
Head-to-head studies in CD and UC – more are needed; the only trials that really change treatment practice / sequencing
Despite options and data, uptake by clinicians is not happening (Siegel CA Clin Trans Gastro 2020)
TREAT TO TARGET
Adjusting therapies until goal achievedChallenges with treat to target
Crohn’s only –
Optimisation of one therapy, not sequencing to other MoA
Timing : how long to wait btwn assessments
How far to go
Need pragmatic research – verdict in UC, perianal, post-opCOMBINATION THERAPIES –
Breaking the therapeutic ceilingPractical considerations
• Due to inadequate response
• Treatment of multiple diseasesMechanistic considerations
• Additive efficacy
• Synergy
• DurabilitySafety considerations
Cost considerationsOn-going combo studies
• DUET UC and CD
• EXPLORER 2.0
• ExiGEM
• Various diet studiesBIOMARKER-DRIVEN – elusive but promising
? will finally come of age with the biomarker in the TL1A studiesConsider clinical clues – cytokine-based strategies
The presence of other IMIDS gives clues to dominant biological process and therefore clues to treatment targetFUTURE CONSIDERATIONS
Emerging endpoints of interest
• Transmural healing
• Disease clearance
• Collateral remission (rheumatology) or functional remissionIn progress STRIDE III (end 2025 / 26)
New(er) and novel treatments
Improving existing MoAs
New MoAs – novel small molecules, mucosal healing agents, cellular immunotherapy
Pulse and de-escalation strategies
Biome-based strategies
Dietary strategies – elimination; modification
Obesity and IBD
by @EdwardLoftus2
Obesity is a chronic inflammatory state
Adipose tissue is not biologically inert (TNFa, IL-6, IL-8, leptin, adiponectin)
Postulated role in the pathogenesis of IBD
Potential risk factor for adverse outcomesTrends in BMI among IBD patients at diagnosis in Olmsted County
Doubling of obesity rates in 20 years in CD and UC (Johnson AM JCC 2021 and J Clin Gastro 2024)Obese patients more likely to have a colonic phenotype; no associations in UC
No consistent relationship between BMI and disease complications in CD
But in UC there was associated increased risk of needed steroids and hospitalisation, but no impact on surgeryCalifornia study showed no association between BMI on hospitalisation or surgery or serious infection (Gu P Am J Gastro 2022)
How does obesity impact IBD therapy?
Not all meds are weight-based
Obese patients less likely to receive optimal weight-appropriate therapy
IFX 4 mg / kg vs 7.9 mg / kg
AZA 1.1 mg / kg vs 1.7 mg / kgHigher IFX levels may be required for patients with higher visceral adipose tissue (Yarur A et al Am J Gastro 2023 Nov : 118)
Higher VAT associated with reduced rates of clinical and endoscopic remission (Yarur Gastro 2023)
VAT may be more informative measure than BMIBariatric surgery is acceptably safe in obese IBD patients (Bazerbachi F Obes Surg 2018)
790 patients among > 300 k who had bariatric surgeryDe novo IBD following bariatric surgery – case study of 42 patients (Braga Net MB et al JCC) and Kochhar GS AP&T 2020 – (lower rates of IBD afterwards)
Impact of bariatric surgery on long-term course of existing IBD
Endoscopic bariatric therapies may be effective in obese IBD patientsAnti-obesity meds may be effective in obese IBD patients (Pham JT Am J Gastro 2024)
No increased risk of AE’s in obese IBD patientsGLP-1 R agonists
No difference in efficacy
Safety appears similarCan they reduce the inflammatory burden in IBD?
Indirect effects: weight loss, glucose metabolism
Direct effects: reduction in pro-inflammatory cytokines (↓ IL-6 and TNFa; blockade of NF-κB signalling; ↑ Treg activity)
Murine models: GLP-1RA decreased colonic inflammation in DSS colitis; ? through modulation of gut microbiota (↑ Lactobacillus reuteri; ↓ enteropathogenic Staphylococcus)5 observational studies published (see figure)
3 / 5 show decreased risk of adverse IBD outcomes, flare, surgery
2 / 5 no difference in IBD outcomesLilly are planning RCTs of Munjaro plus Mirikizumab in UC and in CD – watch this space! #DDW2025
Fatigue and IBD
by Ailsa Hart
Assessment
• Fatigue assessment scale
• FACIT score
• VAS (0-10)Assessment checklist: inflammatory status, lab tests and screening for co-morbid conditions
Then “Do you Sleep?”
Is sleep interrupted by symptoms, or early waking due to depression?Fatigue with insomnia
Non-pharmacological measures:
• Low alcohol and caffeine
• Regular wake time and avoid daytime sleeping
• Increase "pressure" on sleep through increased activity during day and sunlight exposure
• Graded exercisePharmacological measures:
• Mirtazapine (15 mg nocte for insomnia only, 30-45 mg if depressed) & assess in 2-3 m
• Avoid benzodiazepinesFatigue without insomnia – much harder
Avoid Boom and Bust cycles
Plan – prioritise and paceIf appropriate use SSRI / SNRIs
Assess for depression with PHQ-9 – anyone 10 or more has significant clinical depression
Modafinil for fatigue in IBD
Wakefulness-promoting agent affecting specific brain regions (hypothalamus) and neurotransmitters (incl dopamine)Supported by Maudsley guidelines in psychiatry and supported by meta-analysis
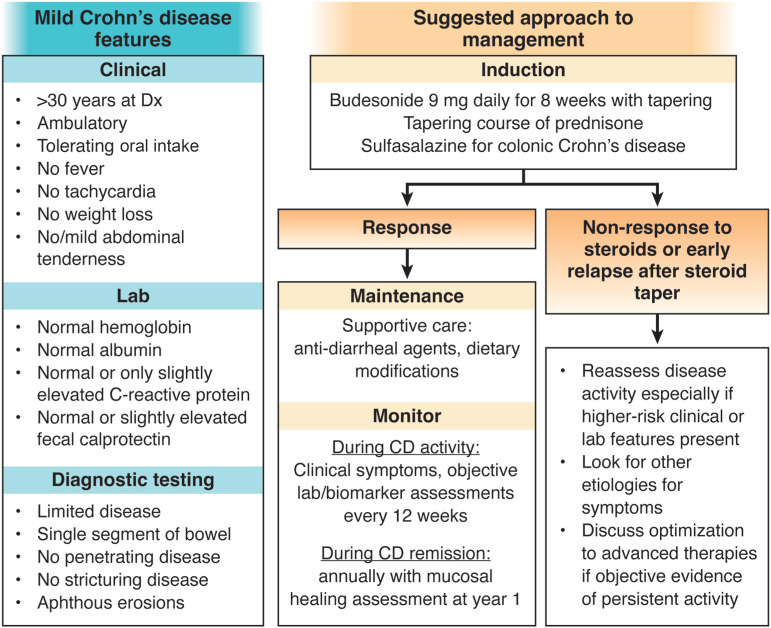
Mild Crohn’s Disease to kick off Day 2
by @ryanungaro
Approx 30 % patients will present with mild Crohn's disease, of whom the majority will maintain a mild phenotype over time
Mild activity and mild severity
But some will progress, so it is important to keep a close eye.
So treat with induction therapy (see figure from Elmasry and Hall CGH 2023) and monitor (nb we do not use sulfasalazine in CD)
Escalate if monitoring indicates transition to moderate or severe disease
Monitoring of Inflammatory Bowel Disease
by Marla Dubinsky #DDW2025
Proactive disease monitoring associated with better outcomes
Treat to target strategy should be the gold standard of IBD management
IUS-driven treatment optimisation leads the way for treating to target
Passive monitoring with wearables and sensors are gaining momentum
Tools to monitor for subclinical disease can give way to disease prevention
Thanks for following along live from DDW 2025
If you’re at the meeting, let me know what’s caught your eye on the IBD track. If you’re following from afar, drop your questions or reflections in the comments. And if this roundup was useful, consider sharing Atomic IBD with a colleague.
— Charlie
P.S. New here? Subscribe for more real-time insights and deep dives on the latest in IBD research, tech, and care.








Thanks this is the most comprehensive summary
Great stuff, thanks for keeping us updated!