I’m in optimistic, yet sanguine mood.
Newly diagnosed IBD patients in 2023 can expect great outcomes.
We have effective drugs, great monitoring tools and extensive data on how to deploy them and what to do when they fail.
But not everyone, and not everywhere.
We are we still failing far too many of our IBD patients.
Our drugs don’t always work - in many cases where we have the evidence, in sub-phenotypes where we don’t and in certain patient populations such as children and the elderly.
And even when we know exactly what to do, all too often we don’t or can’t.
There is a long way to go to ensure equity of care for all people living with IBD across the world. A very long way. And this is something that we should all care deeply about.
These are nine* of the areas where we should focus to make the next breakthroughs:
(*not an exhaustive list)
1. Building a solid evidence base
The basis of all that follows.
We would not be allowed to use a new drug therapy unless it passes rigorous testing in randomised controlled trials. This should apply to dietary and microbial strategies too.
We also need robust data to inform which molecules, diets, bugs, monitoring strategies, etc to take forwards.
2. Fistula and stricture therapy
The failure of mesenchymal stem cells in perianal Crohn's disease (ADMIRE-2) highlights the need for renewed focus here.
Stricture therapy remains almost entirely with mechanical solutions.
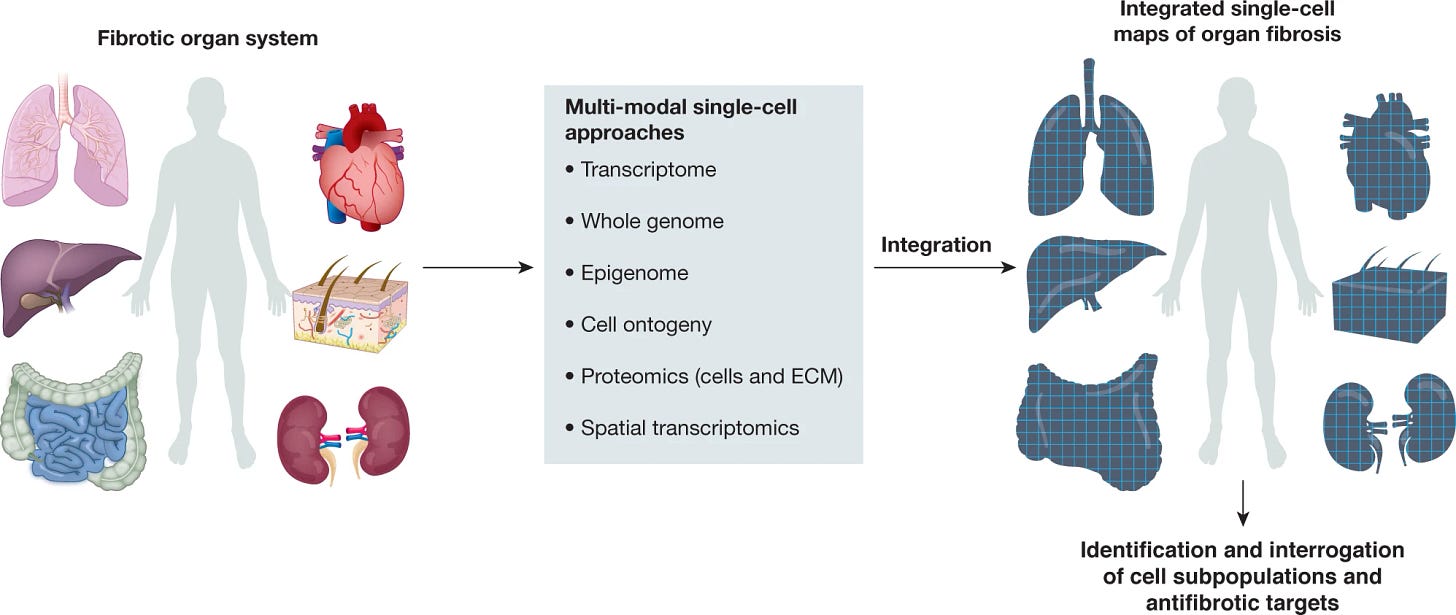
But a coordinated programme of work led by the STAR consortium is, in parallel with efforts in other organ systems, starting to yield the molecular and clinical insights to drive novel therapies.
3. Microbial and dietary strategies
The therapeutic ceiling for IBD is depressing low and we are only nudging it upwards with new targeted drugs.
Progress will come quickly once we layer in microbial and dietary strategies on top of drugs.
It is exciting to see the evidence for dietary emulsifiers in Crohn’s disease evolve rapidly. The basic and translational science has led to the ADDapt trial, which has nearly finished recruiting.
4. Rational combinations of therapies
We hear chat about combination therapy ALL THE TIME So ... what's the big deal?
Learning from other diseases (e.g. viral hepatitis) and our failure of precision medicine, an obvious approach is to target multiple pathways at once. Will it give true synergy? Or will we simply double our changes of getting one right drug to a patient?
For sure the VEGA data are very promising, high quality data.
But most of our experience in the clinic is not in bionaive UC patients. It is in those highly refractory to all medicines. We are then trying to work out which to pair together. It is not so straightforward, and data are really lacking to inform us here
More to come, but RATIONAL design please!
5. Special populations: children especially
There is too big a lag with building solid evidence and gaining approvals for new therapies in children.
Other populations of importance include pregnancy and the elderly.
We exclude many patient groups from clinical trials of new therapies. Overall the research landscape in IBD does not adequately represent our community.
It is good to see this rise up the agenda, see this wonderful review by Seb Shaji and colleagues in Lancet Gastroenterology and Hepatology (ironically behind a pay-wall)
6. Delivery of high-quality care to all patients
Equity of care requires: awareness, prioritisation, funding, and effective systems.
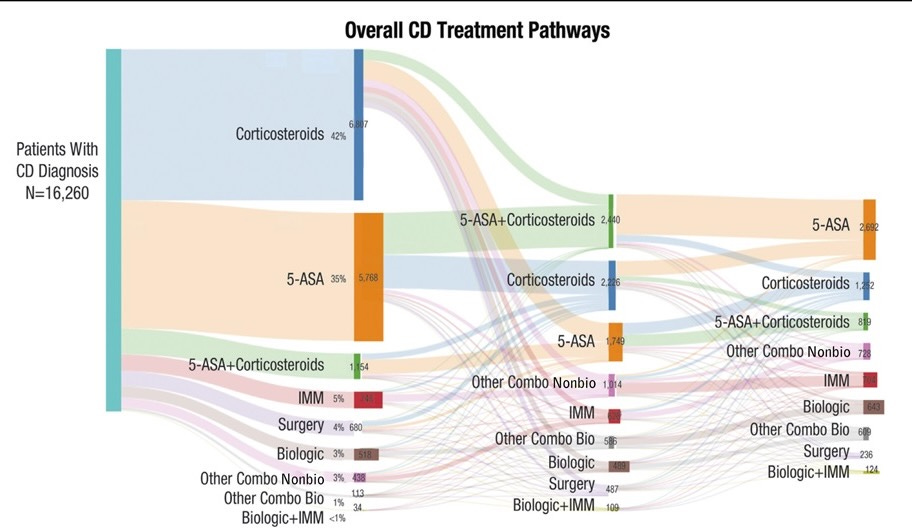
We have miles still to travel here. These data from Corey Siegel on actual treatment sequencing in Crohn’s disease are just staggering:
What’s great though is to see these data drive an analysis of where the systems are failing in order to implement radically new models of care to effect change. The RADIUS hub and spoke model of care is already proving transformative in parts of the USA.
For the rest of the world, I feel we need much more ambitious leadership from ECCO and other key stakeholders.
7. Biomarker discovery to enable precision medicine
We will get there, but it is depressingly slow.
High resolution transcriptomics with single cell sequencing PLUS dynamic biomarker trends over time AND new AI driven analytics will ensure we make progress soon.
Many important studies are ongoing, like IBD-Response in the UK.
8. Psychological and holistic approaches to enhance care
The brain and the gut communicate in a bi-directional manner (see Brain and Body and more intertwined that we knew.)
Therefore we must not neglect the brain in IBD patients.
This means: stress management, optimal sleep, improved resilience, and a focus on diet, relationships, intimacy, work, studies, exercise.
9. Frictionless, passive monitoring that work for patients
Time for true innovation!
If you have diabetes, you can monitor your blood glucose continuously via a patch and via an AI algorithm you can change lifestyle and get the right dose of insulin.
If you have IBD the best we can offer is a faecal calprotectin test at home, or a point of care intestinal ultrasound at the GI clinic.
We can't very well go wondering around with a rectal catheter in, providing continuous calprotectin measurement.
So we need innovation - calprotectin wipes - smart toilets and others I cannot yet imagine. Something for ambitious young founders working across disciplines.










Re FCP monitoring: (1) Would giving collection kits to patients and have those mailed to labs not work? Seems cost and insurance coverage would be the key issues. (2) there are good nanosensors for biologic molecules currently in both universities and in startups. If FCP is durable at room temperature, maybe we could develop a "sensing" molecule that attaches with high specificity to FCP. This approach would take time to develop and test, but unit costs would be neglibly small, and time-to-result would be comparable to other @home strip tests like COVID, urine, pregnancy etc.